
Health Systems & Pandemic Preparedness in Focus at the Global Fund
Author:
Madhuri Kamat
Article Type:Article Number: 5
At the end of last year, the Global Fund review meeting on health systems and pandemic preparedness covered the efforts and results of the work on strengthening them as we enter Grant Cycle 7. The Secretariat’s presentation highlighted key concerns and actions to address bottlenecks so as to ramp up the speed and quality of implementation while acknowledging where they fell short. This article summarises these key points.
Overview
The Global Fund is the largest global multilateral grant funder providing predictable/ long-term (multi-cycle) funding to strengthen key health systems-pandemic preparedness response functions in an integrated people-centred way; while assuring quality services. This has been achieved by an evolving Global Fund strategy, which gets translated into effective grant design to end HIV, Tuberculosis and Malaria (HTM). Strengthening Resilient and Sustainable Systems for Health-Pandemic Preparedness and Response (RSSH-PPR) is part of this framework (Figure 1).
Figure 1. Global Fund Strategy Framework
|
Types of RSSH Investments
|
In the last quarter of 2023, as the Global Fund’s grant cycle entered its 7th replenishment (2023-2025), it was an opportunity to reflect on RSSH-PPR in a review meeting at which the Secretariat made a presentation.
Successes
Delivering on Planned Strategic Activities
The Global Fund Secretariat delivered all planned strategic activities to improve the quality and quantity of RSSH-PPR funding requests: policy and systems incentives; country engagement/dialogue; and technical support with prioritization in selection of essential RSSH-PPR areas in each focus country and intentionally securing funding for the same. At the same time there was a push towards enhancing holistic planning of Grant Cycle 7-Covid 19 Response Mechanism (C19RM) towards strengthening key RSSH-PPR functions.
Scale-Up in RSSH-PPR Investments
Grant Cycle 7 (GC7) added to C19RM’s resources enabled likely the most significant scale-up of the RSSH-PPR investments in the GC7 period (Figure 2).
Figure 2. Scale-Up of RSSH-PPR Investments in Grant Cycle 7
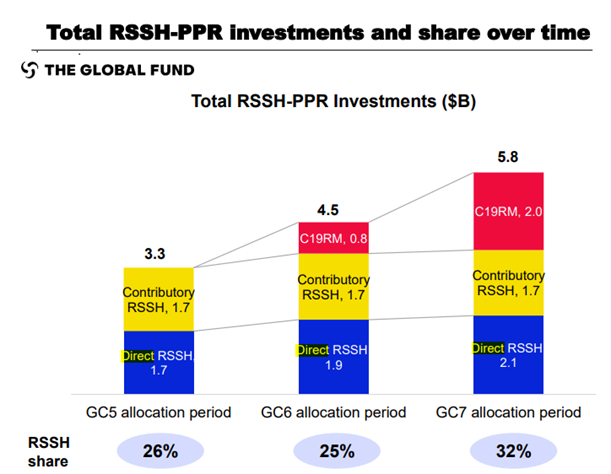
Country Coordinating Mechanisms (CCMs) are rationally using the C19RM to resolve the tension between increasing RSSH investment and sustaining investment levels across the diseases as funding for them flatlined. In Mali, for instance, reinvestment of the C19RM will allow for increased multi-disease testing capacity, through the establishment of a computerized national logistics management information systems interoperable with the district health information system. Portfolio optimization will include strengthening the decentralization of diagnosis and the development of a national plan for integrated sample transportation and a national multi-risk action plan. These will go hand-in-hand with capacity building training across all levels with quality assurance and improve analysis of data to monitor and respond to public health emergencies.
Positive Trend for Human Resources for Health Strategic Investments
There was an overall increase in the supervision of human resources for health, training and governance investments. A preliminary analysis of a sample of 31 RSSH priority countries showed a growth in support to maintaining a pipeline of health workers and in the quantity and quality of community health workers’ investment. There was also good uptake of new, more evidence-based interventions.
Enhanced intentional RSSH-PPR investments in target areas
As compared to the GC6, in GC7, countries fully utilized the matching funds they were eligible for and doubled budgets for human resources in health and lab systems. This in turn led to the strengthening of health systems’ human resources (in areas of governance, data and analytical capacity to plan for their better deployment, distribution, performance and retention) and better lab systems (including sample transport, diagnostic network optimization and lab data systems). Targeted health facility assessment planning is also on track to measure their integration, people-centered care and other key results for C19RM and GC7.
Implementation Snafus
Diffused Focus
The slow uptake of investments by countries in the GC6 as compared to GC7 was the result of fragmentation across donors and agencies, with no functional coordinating and accountability mechanisms or link to robust national plans. Furthermore, RSSH-PPR entities are not leading implementation and hence, RSSH investments get divested from programmatic focus. Technical assistance remained uneven or delayed and is often driven by the priorities of the donor rather than of the country. Administrative hurdles may also have blocked, for instance, integrated laboratory systems strengthening.
Poor Monitoring and Evaluation
RSSH indicators were poorly defined without clear linkage with investments, and were not used for Performance Frameworks in GC6.
Capacity Challenges
A potential 2 billion USD for C19RM available funding, combined with GC7, enables approximately a third of the entire funds to be available for RSSH-PPR activities during the GC7 period. Hence, it is implementation capacity, rather than insufficient funds, which is the key constraint at present.
Accelerating Implementation
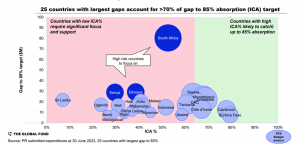
In response to the above bottlenecks, direct RSSH for GC7 demonstrates more targeted and less fragmented investments than past cycles. Further, during GC6 itself, a very targeted engagement was initiated with high-risk countries to accelerate implementation (Figure 3).
Figure 3. In Country Absorption (ICA) Gap, 6th Replenishment Cycle
Review of contributory RSSH investments
In GC6 most contributory RSSH came from TB and TB/HIV grants with largest cost inputs being salaries and training. The share of contributory RSSH increased from 12% in GC6 to 13% in GC7 and is set to increase further with potential additions to contributory RSSH for activities that contribute to systems beyond a single disease. These could include, to name a few, comprehensive sexual education and social protection interventions (HIV), reforming policies, regulations and laws (TB); intensified activities for elimination and post-discharge chemoprevention (malaria).
Best Practices in RSSH
|
Mozambique’s strong leadership at the ministerial level and within the CCM saw a significant increase (22%) in RSSH investments in GC7 and is likely to also receive C19RM funding for RSSH activities. Their inclusive planning process of funding request design and grant-making is a strength and grant-making is focusing on facilitating further integration opportunities across the RSSH spectrum. During GC6, Secretariat set-up quarterly meetings in Mozambique for RSSH workplan review. Each Directorate receiving RSSH support prepared quarterly reports against the milestones to submit to the Secretariat for review in facilitating further integration. |
|
Indonesia created an ambitious health transformation roadmap to strengthen RSSH and expand integrated primary healthcare services. Indonesia increased provincial and district government capacity to develop health workplans/budgets that correspond to minimum standards, including for the three diseases, and enhanced involvement of multisectoral parties in their development. Indonesia introduced a hub-and-spoke model for whole genome sequencing and bio-banking at the district level. A “one health” platform consolidates health information by integrating all disease-specific data systems. Rigorous in-service training and integrated supportive supervision and human resource planning and management were undertaken, which will contribute to the effective scale up of IPCS from 9 to 40 districts in GC7 increasing disease coverage services at the community level. |
Closing the Gaps
Focus on improving quality of HRH investments and value for money:
The Technical Review Panel called for more human resources in health investments, and aligning community health workers with the broader human resources for health policies and budgets so that they are not reduced to just filling gaps at the primary health center level. The Secretariat recommended among others things, use of health labour market analysis, and development of time bound agreements to aid transition. There is also a need for more deliberate approaches to tackle the continued high reliance on ad hoc training.
Measuring contributory RSSH:
There is a need to undertake an external review of the contributory RSSH methodology/definition as well as a deep-dive review in a few countries with high contributory RSSH investments to examine activities and explore other approaches to strengthen their systems contribution.
Making it Work
|
Post-Covid Strategic Priorities
Action Points
|
Monitoring and Evaluation
RSSH monitoring in GC7 is being strengthened with better uptake and use of RSSH indicators. The RSSH pandemic fund dashboard maps out dollar investment and its indicators for each country and module, to systematically highlight gaps in pandemic fund indicators for country dialogue. Additionally, the GC7 will target and measure systems strengthening in digital management information systems, surveillance, supply chains and laboratories and the pilot models will be rolled out in selected priority countries.
What Lies Ahead?
Learning from the Best Practices, the Global Fund will also invest in national plans and coordination mechanisms beyond the program management units. By investing directly in national plans, it shows the Global Fund’s willingness to be more enabling in facilitating country ownership, a longstanding sticky point between countries and the Global Fund. Yet, it may also indicate potential problems as programmes usually get allied to the government of the day and may also invite a backlash at some point that the Global Fund’s weighty investment is influencing the direction of the plans. Countries were nudged, for instance, towards a co-financing policy to enhance domestic spending for RSSH-PPR; including additional priority needs, based on their national action plan for health security.
It is pertinent to note that the reservations of an exclusive focus on the direct RSSH investments leading to missed opportunities to broaden disease-specific investments is already on the agenda of an upcoming Global Fund session. Taken together with the Secretariat’s admission to its low bandwidth for monitoring and oversight of the implementation of RSSH investments, the Global Fund needs to acknowledge what countries have been saying all along – that a centralised single-point, one-size-fits all focus for monitoring and evaluation does not work. The findings of the Multilateral Organisation Performance Assessment Network’s review of the Global Fund’s performance in 2021-2022 stated as much when it called upon the Global Fund to “make more progress” on RSSH-PPR and a “cohesive and fully independent evaluative function” that apart from simple monitoring allows more in-depth learning and understanding from the programmes it supports. It also pointed out that country ownership and stakeholder priorities competing for attention will be up for discussion in the coming years.
