
A Leap of Faith and a Career-changing perspective: Notes from the Zero TB Field Diary 2017
Author:
Julia Bürgi
Article Type:Article Number: 9
Julia Bürgi reminiscences on the career shift she took in 2017, which altered her outlook on how global health work, particularly in TB, is represented on paper at the global level compared to the reality of its implementation. In a frank assessment, she acknowledges that having lived and been educated in North America and Western Europe, the field-level learning from diverse settings in Asia and Africa enabled her to develop a more grounded perspective on the hard choices presented to implementers and health care providers.
It was 2017 and I was taking a leap of faith of sorts, leaving a cozy staff job at The Global Fund for a small global health organization that worked primarily on urban-level tuberculosis (TB) planning and human immunodeficiency virus (HIV) harm reduction for people who use drugs. As I departed, I told colleagues, friends, and family that I was eager to move from writing reports about global health and instead, “do the work that other people will write about”. My new employer was Advance Access & Delivery (AA&D) and my role was to support their Zero TB Cities project with infection prevention and control technical expertise. I had been working in global health for a scant 3 years and spent the vast majority of my life in North America and Western Europe so I entered my new job with passion, but also a strong dose of naivete and white saviorism.
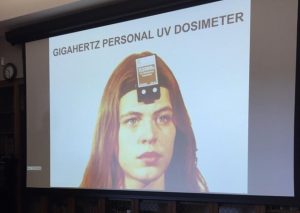 The course “Building and Engineering for Airborne Infection Control” at Harvard Medical School covered safe use of methods such as germicidal ultraviolet (UV) lights. This picture shows the mechanism that measures the strength of a UV lamp. |
I had spent the summer of 2016 learning about infection prevention and control at a course hosted by Harvard Medical School and the U.S. Center for Disease Control to prepare for my job change the following year. Infection prevention and control involves personal protective equipment (such as face masks), spatial interventions (such as hospital layouts), and administrative interventions (such as hand washing protocols for doctors and nurses). Prevention and control of airborne infections, such as TB, require focus on air cleanliness and filtration, unlike other diseases that spread through surface contact or bodily fluids.
It is to be noted that today airborne infection prevention and control practices are much more common as the result of the COVID-19 pandemic, which, like TB, spreads through the air. However, in 2017, this was still a niche corner of public and global health.
My fellow students at the Harvard course included members of the Cambodia Ministry of Health, the on-the-ground manager of Mongolia’s Global Fund-supported TB programs, healthcare architects from Rwanda, and a medical equipment engineer from India. I listened to their comments about top-down urban planning practices to make way for new hospitals in Addis Ababa, Ethiopia; and the politics of publishing infection prevention and control guidance within the World Health Organization regional offices. I remember being surprised to hear about how onerous reporting requirements from global health funders were, as well as the skepticism that the course curriculum could be feasibly implemented.
For me, the most exciting part of the new job with AA&D was that it took me from behind a computer and put me in touch with the communities delivering and receiving TB care around the world.
 On a visit to the home of a child being treated for pediatric multi-drug resistant (MDR-) TB in Chennai, India, I saw, for the first time, the medicine taken by MDR-TB patients and tactics for managing its frequent administration. |
During my time with AA&D, I traveled to Chennai, India and Durban, South Africa and held regular calls with Zero TB Cities’ partners in Kisumu, Kenya; Karachi, Pakistan; Ho Chi Minh City, Vietnam; and Lima, Peru. I often recalled the challenges explained by my fellow infection control students the year prior, which had felt so abstract to me at the time but all-too-clear as I advised Zero TB Cities’ project partners. Looking back, the reports I had written for The Global Fund from Geneva had, of course, used correct terminology and were viewed by dozens of colleagues to ensure accuracy. Nonetheless, my careful writing inherently reflected a sanitized and distanced understanding of health care delivery in countries beyond my personal experience. My new work was educative and even shocking sometimes, with every experience demonstrating that good quality infection prevention and control work was much messier in practice than on paper.
 This diagnosis and x-ray center in Chennai, India relied on an air conditioner for climate control that did not sanitize or filter the air. This recirculated air potentially carrying TB particles by patients with a persistent cough being x-ray screened for TB. |
During visits and calls, I had exchanges with municipal officials, community health workers, and hospital infection control administrators who asked questions that required me to reconfigure and synthesize in a way that report-writing had not demanded of me. I was asked, “Do I need to change my clothes after delivering medicines to patients with multi-drug resistant TB to avoid the possibility of infecting my family?”. Yes, in theory, clothing could hold TB particles that could be shaken loose into the air, but this would be an unlikely way for TB to be transmitted and this would also depend on the level of exposure a healthcare worker had to the patient’s coughing and how well aerated the clothing was on the health worker’s way home. If a healthcare worker practised optimal distancing and use of personal protective equipment at all times, then the risk was extremely low or nonexistent. If everyone behaved according to guidelines in the real world, though, there would be a lot less disease. A healthcare worker might end up very close to a patient to bring the patient water or food, or could help up a patient who has collapsed. This makes ideal practice, quite understandably, much easier said than done.
Another question that stumped me: “If my TB program has a limited amount of money, do I prioritize paying for the staff to be trained in infection control or purchasing face masks?”. In the case of prioritization between training and personal protective equipment, each activity – in theory, yet again – is of equal importance and both of the absolute highest priority. The absence of one would compromise the safety of anyone in a high transmission risk space. Personal protective equipment used incorrectly is nearly pointless, but so is training staff on its correct use without being able to then give them the equipment to use. The question I ended up asking myself is how and why healthcare providers were being put in the position to make such impossible decisions.
 Caption: The pathway for patients to enter a hospital campus in KwaZulu-Natal, South Africa was open air with protection from rain. However, the hospital’s waiting room was an enclosed room in the center of the building with no external ventilation, risking the spread of airborne disease between patients in that space. |
Then there was the matter of advising on spatial interventions in healthcare delivery spaces. A certain spatial layout can effectively prevent TB from going from, for example, a coughing person to someone with a broken arm, or the nurse treating them both. Correct practice, in theory, means avoiding use of wall-mounted air conditioners that cool but do not filter air, or bring in outside air. However, in cities such as Chennai, Durban, or Karachi that suffer from air pollution and regularly go over 32 degrees Celsius/90 degrees Fahrenheit (or similarly extreme cold temperatures in winter), this is another case of “easier said than done”. A doctor’s or hospital’s waiting room without air conditioning – even when substituted with windows and fans – will simply prevent patients from coming in or put patients at risk for ingesting air pollution or experiencing heat stroke. Even if a health care provider is open to the possibility of spatial changes, they may be too costly to implement, such as in the case of a hospital in Durban. At this hospital, the waiting room for coughing and non-coughing patients alike was a windowless room on the interior of the hospital with wall fans that depended on intermittently available electricity and no form of ventilation filtering or bringing in outside air. This hospital’s Chief Nurse, who also served as the head of infection prevention and control, said the hospital administration would be unwilling to relocate the waiting room to an outdoor or building periphery space with windows, or pay for additional staff resources to triage patients based on coughing to sit in a separate area.
I was also keen to take an urban-level perspective and was met with the challenges of informality and security. I suggested to colleagues in Kisumu, Kenya that the buses (known locally as matatus) be given stickers encouraging people to open the windows to ventilate during long commutes. These colleagues were kind enough not to laugh at me, but when I visited Kenya for the first time a few years later, their feedback finally made sense: Matatus are not owned by a single company nor formally supported by municipalities. It would be like herding cats to ask them all to put stickers on the insides of their vans, trucks, and buses. Furthermore, open windows could become a security issue, with passengers vulnerable to grabby hands from outside the bus. On this first trip, I had a little laugh to myself about how well-intentioned but infeasible my idea several years earlier had been.
 Pharmacies in Chennai, India are typically a walk-up window that keeps patients outside and pharmacists inside. This design is meant to keep operating costs low for pharmacy owners, but unintentionally protects pharmacists from the risk of contracting TB and other airborne diseases. |
My time working in infection prevention and control was eye opening and, at times, I worried that the communities I was seeking to support were giving more to me than I was to them. Nonetheless, I was able to help make changes here and there, or validate when infection prevention and control was being practised well.
 The view from the backseat of a taxi in Chennai, India. I often spoke with taxi drivers in the places I visited, who nearly always had first-hand stories of a family or friend with TB and were eager to share their experiences. |
Ultimately, I was gifted with a more humane understanding of global health informed by more than my own healthcare seeking incidents in the US and Western Europe or what is in a neatly printed report. It was also the individual stories – the ones that numbers in reports don’t tell – that crystalized the importance of work in global health and, at the same time, the inability for it to be transformed overnight. While no single experience (or handful of experiences) can be universally applied to other people, places, or circumstances, I was humbled to discover a fraction of the ways in which healthcare delivery varied from my perspective up until that point. I have taken this to heart and head alike and since then I have and will always carry this with me across my future work in global health.
