
When the South commits suicide to heal the North. About international recruitment of healthcare professionals
Author:
Christian Djoko and Ekelru Jessica
Article Type:Article Number: 4
The international recruitment of nurses by wealthy countries is a phenomenon that has gained momentum in recent decades. Developed countries, faced with an aging population, growing demand for healthcare services and a shortage of nurses, are increasingly turning to developing countries to fill the gap. This practice has a profoundly negative impact on the healthcare systems of African countries, which often lose their qualified nurses to wealthier countries.
Background and reasons for international recruitment
Developed countries, particularly those in North America and Europe, are facing a healthcare workforce crisis. The aging of the population, the increase in chronic diseases and the difficult working conditions have led to a shortage of nurses. To fill this gap, these countries have implemented aggressive international recruitment policies, targeting mainly developing countries where the cost of training nurses is lower, and where economic conditions are driving these professionals to seek better opportunities abroad. While this movement offers individual opportunities for migrant nurses, it also has complex consequences for the healthcare systems of the countries of origin.
Site surveys
Developed countries, particularly those in North America, Western Europe and parts of Asia, have been facing a growing demand for healthcare in recent years, due to aging populations, the rise in chronic diseases, the COVID-19 pandemic, difficult working conditions, advances in medical technology and heightened expectations in terms of quality of care. This demand has exacerbated the shortage of qualified nursing staff, prompting these countries to actively recruit abroad. According to a study by Global Burden of Disease, (GBD) the number of nurses and midwives available in 2019 was 29.8 million (with a 95% uncertainty interval ranging from 23.3 to 37.7 million) and the global shortage of nurses and midwives was estimated at 30.6 million, four times higher than the 7.5 million estimates produced by the WHO, although these figures are based on different definitions (Figure 1).
Figure 1: Different estimates of the nursing shortage: WHO and Global Burden of Disease (GBD)
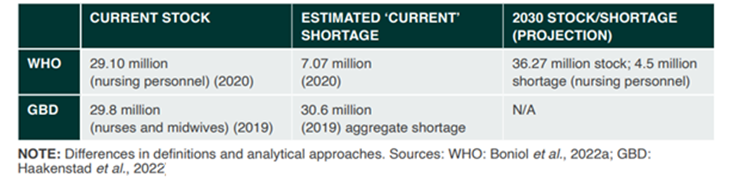
Source: Recover to Rebuild Report of the International Council of Nurses, 2023: p.15
Around 80% of international migration of nurses is mainly initiated by seven or eight wealthy countries, including Great Britain, the USA and Canada (Figure 2). These countries implement attractive policies and programs, offering financial incentives, career opportunities and relocation facilities to attract qualified nurses from developing countries in general and Africa in particular.
Figure 2: Selected OECD countries, percentage of foreign-trained nurses, most recent year
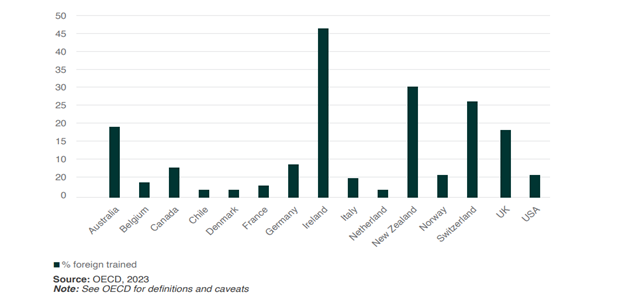
Source: Recover to Rebuild Report of the International Council of Nurses, 2023: p. 44
In 2020, the WHO published a red list aimed at preventing wealthy countries from poaching healthcare workers from countries where there is a shortage of healthcare personnel. The list includes Nigeria, Ghana, Zimbabwe and 34 other countries in the African region. Despite the existence of this list, over 2,200 new foreign nurses registered in the UK (or 20%) between March and September 2022, came from Nigeria and Ghana. Data from the Ghana Nurses and Midwives Association shows that nearly 4,000 nurses left the country in 2022, while in Zimbabwe, more than 4,000 healthcare workers, including around 2,600 nurses, left the country in 2021 and 2022, the Zambian government revealed.
In the French-speaking African region, it’s the same story. Daniel Boily and David Gentile for Radio Canada in “The African sector to recruit 1000 nurses” on March 1, 2023 reported that Quebec has invested heavily in the active recruitment of nurses in Africa, offering scholarships of $65,000 per nurse. By 2025, some 1,000 students recruited from Africa (Cameroon, Mauritius, Morocco, etc.) should have completed their training to become nurses in Canada’s largest French-speaking province.
While this movement offers individual opportunities for migrant nurses, it also has complex consequences for the healthcare systems of the countries of origin. Although they sometimes have robust nursing training programs, African countries suffer from economic constraints that limit their ability to offer competitive salaries and attractive working conditions. This disparity prompts many nurses to seek opportunities abroad to improve their living and working conditions.
Consequences for African countries
The international recruitment of nurses raises fundamental ethical concerns.
Loss of skills and manpower
The migration of nurses represents a substantial loss of skills and experience for health systems in developing countries. Let’s take the case of Nigeria once again. According to the Recover to Rebuild Report of the International Council of Nurses, 2023 authored by James Buchan and Howard Catton, projections based on population growth from 2016 to 2030 for this West African country indicate that there could be a shortfall of 140,000 nurses and midwives in 2030 compared with 2016, a shortage of 29%. In Cameroon, one of the countries targeted by Quebec’s first recruitment phase, there are just 0.55 doctors, nurses and midwives per 1,000 inhabitants, and this ratio fell between 2008 and 2018. This contrasts sharply with Canada, where there are 14.2 healthcare professionals per 1,000 inhabitants.
Singularly, migrant nurses are often among the most qualified and experienced, exacerbating the shortage of skilled personnel in local hospitals and clinics. In addition to the shortage created, this assisted flight of qualified nurses from the global South results in an increased workload for the remaining healthcare professionals, a continuous cycle of burnout, a high risk of medical errors, a reduction in the quality of care provided, and even a multiplication of medical deserts. Regions with a low ratio of nurses to population inevitably record higher mortality rates, particularly among mothers and children. Needless to say, infectious diseases such as HIV/AIDS, tuberculosis and malaria are also harder to control without adequate nursing staff.
The recruitment of healthcare professionals in Africa not only compromises the quality of care provided to patients, it also creates an imbalance between rich and African countries in terms of access to healthcare.
Worsening health inequalities
The departure of qualified nurses also has a domino effect on the training and education of new generations of healthcare professionals. Experienced nurses often play a crucial role in the clinical training of student nurses. Their absence inevitably reduces the quality of teaching and practical preparation of new graduates, creating a vicious circle of under-qualification and continued emigration. In Uganda, for example, nursing training programs have suffered from the loss of qualified instructors, slowing down the training of new nurses and exacerbating the shortage. In Zimbabwe, the migration of medical staff has contributed to the closure of some rural clinics, leaving entire communities without access to essential care.
This exodus of nurses to rich countries, this brain drain and skills drain, whatever we may think of it on an individual level, has a negative impact from a systemic point of view. It leads to a significant loss of human capital and a weakening of local healthcare systems.
By recruiting experienced nurses from poorer countries, wealthy nations are effectively externalizing training costs, acquiring qualified nurses at lower cost without offering compensation. In other words, when these health professionals leave their countries of origin, not only is the state’s investment in their training lost, but it also has to bear the additional costs of training and recruiting new staff. This migration of skilled human resources therefore inflicts a double financial burden on African countries, compounding the challenges already facing their healthcare systems.
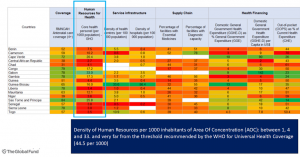
In a podcast with Radio France Internationale on March 17, 2024, the Executive Director of the International Council of Nurses, Howard Catton, rightly asserted that this situation gives the feeling of being part of a form of neo-colonialism: high-income countries use their economic power and wealth to take what they need from more fragile countries. They are creating a new form of dependency that is worrying in the long term, as it stands in the way of the development of universally accessible healthcare systems.” (Figure 3).
Figure 3: Performance of health systems in West and Central Africa: a diverse landscape in the region with notable weaknesses in the system
Socio-economic impact
With regard to the socio-economic impact of this recruitment, it’s worth remembering that Africa, in 2023 represented 18.3% of the world’s population and as reported in 2016-2017, the WHO stated that this region carries the highest burden of disease – 25%. What does this mean in socio-economic terms?
According to WHO estimates published in its report in March 2019 the population of 47 countries across Africa lost 630 million years of healthy life in 2015 to diseases and epidemics. This translated into a cumulative annual loss of more than $2.4 trillion from the region’s gross domestic product value by 2019. The situation is exacerbated because as per the WHO, “the African region carries the highest burden of public health emergencies globally, with over 100 major events reported each year, which include disease outbreaks of Ebola, cholera, measles, yellow fever, meningitis, and monkeypox.” A research study confirmed an average of 102 public health events being reported annually in the WHO African region between 2001-2022. Moreover, a World Bank-published report in conjunction with WHO and other GHIs on Universal Health Coverage: A Framework in Action, 2016 highlighted the fact that per capita out-of-pocket spending, which more than doubled from $15 in 1995 to $38 in 2014 ended up impoverishing 11 million people in the region every year. And 14.4 million people in low- and middle-income countries in Africa fall into poverty annually as a result of rising healthcare costs from out-of-pocket payments.
Hollowing out health systems
The Global Fund, the Lusaka Agenda, and all the Global Health Initiatives (GHIs) agree that there can be no satisfactory results or progress towards the eradication of HIV, tuberculosis and malaria or the achievement of the Sustainable Development Goals (SDGs) by 2030, without the crystallization of resilient and sustainable health systems (SRPS). However, a crucial question arises in the context of massive migration of healthcare professionals to Northern countries: how can developing countries’ healthcare systems be strengthened when their qualified nurses are attracted by better opportunities abroad? How can we hope to establish PRHCs without a sufficient number of qualified nurses? This situation highlights a paradoxical contradiction: Western countries, which are the main donors to global health initiatives, risk undermining the very health foundations they officially seek to strengthen. By draining critical human resources from the health systems of developing countries, these nations are indirectly contributing to the weakening of the health infrastructures they claim to seek to consolidate. It is imperative to resolve this contradiction to ensure that the global objectives of public health and development can be achieved, by striking a balance between the needs of wealthy countries for healthcare personnel and the need to maintain robust, autonomous healthcare systems in developing countries.
Solutions
To mitigate the negative effects of nurse migration, in 2010 WHO adopted a Global Code of Practice for the International Recruitment of Health Personnel. A key statement in this non-binding instrument affirms that: “Member States should discourage the active recruitment of health personnel from developing countries facing acute shortages of health personnel”. However, the implementation of this mechanism has very often proved ineffective. Hence the need to strengthen it.
In addition, it is imperative to strengthen local healthcare systems in Africa to counter the brain drain to wealthy countries. This requires increased investment in several key areas. First and foremost, investment in the education and further training of nurses is essential. Scholarships, international exchange programs and professional development opportunities need to be put in place to encourage nurses to stay and contribute to strengthening local healthcare systems.
These initiatives need to be complemented by policies to improve nurses’ working conditions, offering safe working environments, reasonable working hours and clear, motivating career prospects. Increasing salaries is also crucial to making local positions more attractive and competitive with opportunities abroad.
It is also essential to provide African healthcare facilities with better equipment and resources. This includes not only basic medical supplies, but also access to modern technology and quality infrastructure. A well-equipped and well-supported working environment can greatly improve job satisfaction and nurse retention.
To complement these efforts, partnerships with international institutions and NGOs can be developed to facilitate exchange programs and international collaborations. These partnerships can offer opportunities for advanced training and technical expertise, while strengthening local capacities.
Ultimately, curbing or containing the recruitment of healthcare professionals in Africa requires a holistic and sustained approach, integrating financial investment (as we’ve said on several occasions, notably in this evocatively-titled article: It’s time Africa finances its own healthcare and advancing health financing and universal health coverage in Africa: the role of civil society), supportive policies, and international collaborative initiatives. Only such an approach can create an environment where nurses feel valued and motivated to stay and contribute positively to the health of their communities.
Conclusion
The international recruitment of nurses by wealthy countries has far-reaching and often harmful consequences for the healthcare systems of developing countries. While the opportunities offered to migrant nurses are undeniably beneficial on an individual level, the social and health costs for the countries of origin are high. Concerted strategies, including effective retention policies (increased domestic health funding), equitable international partnerships and ethical recruitment regulations, are essential to mitigate these negative impacts. It is crucial that developed countries recognize their shared responsibility in this phenomenon and work towards solutions that are sustainable for all.
