
Country Alignment for Global Action Plan for Healthy Lives and Well-being for All – A Work in Progress
Author:
Madhuri Kamat
Article Type:Article Number: 5
The World Health Organization (WHO) brought out the 2024 Progress Report on the Global Action Plan for Healthy Lives and Well-being for All, which had been launched in September 2019 at the United Nations General Assembly. It showcases the collaboration betwixt the WHO and other global agencies and health institutions who came together with a broad commitment to implement the Global Action Plan. The report makes specific reference to the impact of country alignment towards this. This article offers some of the significant points made in the report and does not cover it in its entirety.
In the run-up to the 77th World Health Assembly, the World Health Organization (WHO) published the 2024 progress report with a specific focus on “aligning for country impact” vis-à-vis the Global Action Plan for Healthy Lives and Well-being for All (SDG3 GAP).
Overview
The SDG3 GAP is a set of commitments (Figure 1) by 13 international agencies (Figure 2) that have a significant presence in health, development and humanitarian response across the globe. They came together along with the WHO to help countries advance progress on the targets related to health vis-a-vis the Sustainable Development Goals (SDGs) through stronger collaboration.
Figure 1: SDG3 GAP Commitments

Figure 2: SDG3 GAP Agencies
|
Gavi, the Vaccine Alliance; Global Financing Facility for Women, Children and Adolescents (GFF); Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund); International Labour Organization (ILO); Joint United Nations Programme on HIV/AIDS (UNAIDS); United Nations Development Programme (UNDP); United Nations Population Fund (UNFPA); United Nations Children’s Fund (UNICEF); Unitaid; United Nations Entity for Gender Equality and the Empowerment of Women (UN Women); World Bank Group; World Food Programme (WFP); and World Health Organization (WHO). |
There are 69 countries (Figure 3) who use the SDG3 GAP approach covered by the WHO regional offices, namely, Africa (AFRO), Americas (AMRO), South East Asia (SEARO). Europe (EURO), Eastern Mediterranean (EMRO) and West Pacific (WPRO).
Figure 3: SDG3 GAP Usage across Countries grouped as per WHO Regional Offices

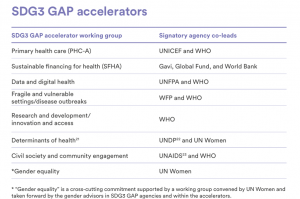
The SDG3 GAP covers thematic areas for which joint support is extended to countries by agencies. These thematic areas with gender equality as a cross-cutting issue are critical for attaining health-related SDGs (Figure 4).
Figure 4
In the following sections, we dwell on some of the significant points made in the report.
Accelerating on Primary Health Care
Make a stronger contribution to primary health care (PHC) by effectively strengthening systems for health, with integrated delivery of services aligned behind one national plan – Lusaka Agenda.
The Primary Health Care accelerator (PHC-A) approach has three components, namely, recognizing primary care and essential public functions as the core of integrated health services; multi-sectoral policies and actions; and recognizing the power of people and communities. What the PHC-A does is to bolster countries who must develop and deliver the comprehensive package of essential health services through this approach with the end-goal being Universal Health Care for all. What is to be noted is that prior to the PHC-A, there was no other platform for inter-agency coordination for primary health care. The reason why it has worked well in the 20 countries using it is primarily because it received “good traction” as per the report from both agencies and development partners with the partners meeting monthly in the initial four years of the initiative.
The platform besides being for inter-agency coordination also does much more: it provides mechanisms for experiential learning between countries, for example, lessons from primary care networks in Kenya at the subnational level have been shared with Malawi’s Ministry of Health. It also addresses challenges and identifies opportunities for sustainable country impact. This took place through country dialogues (Figure 5) on specific thematic areas tailored to each country’s unique needs as well as separate thematic discussions for strengthening health systems (funding and monitoring and evaluation (M&E) mechanisms; integrating COVID-19 response efforts with existing PHC initiatives; and water, sanitation, and hygiene (WASH) in health-care facilities).
|
Figure 5
|
The SDG3 GAP now also includes elements of Every Woman, Every Child (EWEC) in primary health care, which will allow for more cohesive integration of sexual and reproductive health and rights (SRHR) and women’s, newborn and adolescent health into primary health care. This expansion is welcome given the criticism that SRHR is often overlooked in the focus on the latter.
The success of the PHC accelerator underlines how important it is not only to have a shared commitment to attaining goals but how to shape a shared consensus on how to go about it through constant engagement with countries allowing them to determine their priorities within an overarching framework.
Operationalizing Engagement
Best Practices in country-specific collaborations included having clear principles for partner alignment; using a formal agreement or operating framework between government and development partners for development assistance; having a health sector strategic plan around which partners can align their support to countries; ensuring alignment with essential health packages that are part of national plans; using existing national health coordination mechanisms; doing joint planning and joint programming (Belize, Ethiopia, Malawi, Maldives); using pooled donor funding or funding to support an agreed national plan (Côte d’Ivoire, Ethiopia, Honduras); and building mutually respectful relationships among development partners and between development partners and national governments.
Successful collaborations included strengthening of institutional frameworks by establishing a health sector coordination mechanism (Côte d’Ivoire); the ministry of health playing a role in ensuring a certain level of coordination for support received (Jamaica); having a national team responsible for SDG3 (Jordan); using a coordination mechanism between the ministry of health and partners, with regular meetings and thematic technical working groups (Mozambique) — coordinating through technical working groups to align partners’ support (Sierra Leone). The Madagascar example (see below) showed how reviving the coordination mechanism for national health systems with funding support and clear mandates for committees can accelerate progress towards fulfilling SDG goals.
|
Madagascar Case Study Problem Identified: Madagascar’s Ministry of Health (MOH) highlighted the complexity in aligning the activities of its technical and financial partners, which include SDG3 GAP partners (UNFPA, UNICEF, World Bank, Global Fund, Gavi, and WHO), with the government’s health-care priorities. Engagement: Based on the survey results, WHO initiated informal discussions with key technical and financial partners to revitalize the Strategic Health Sector Coordination Platform. Funding support: By 2023, catalytic funding from the SDG3 GAP Secretariat also provided essential financial support (US$ 20 000 in 2022 and US$ 50 000 in 2023) to strengthen coordination mechanisms and advance work on MOH-led prioritized technical areas. Setting Country Priorities: In March 2023, the Ministry of Health and technical and financial partners held a coordination meeting to discuss health priority setting and alignment. These priorities included accelerating the fight against neglected tropical diseases, HIV control with a focus on people who inject drugs, as well as reducing maternal mortality through improved emergency care. Committees facilitate collaborative strategic planning and promote enhanced cooperation among stakeholders within the national health sector. |
Great Expectations?
The 2024 Progress Report on the Global Action Plan for Healthy Lives and Well-being for All points out that collaboration across the health ecosystem requires governing bodies of the agencies as well as other accountability mechanisms to sign on to investing for human and financial resources but the bugbear of “resource constraints” and the core mandates of the respective entities means it’s a bridge too far. And also makes more challenging the necessity of actually going beyond the minimum expectations and forging deeper collaborations. As pointed out in the reflections of some co-leads mentioned in the report, it is the already funded, functioning workstreams that got a value addition by being part of the SDG3 GAP. An example is the Sustainable Financing for Health accelerator, which has Gavi, Global Financing Facility and the Global Fund who had collaborated on a 4G initiative, co-leading it with the addition of the WHO. However, there are also other issues around making collaborations actually work operationally. For example, the accelerator for Research and Development, Innovation and Access, has not has not had a single meeting in 2023. So, it’s a mixed bag on whether agencies, which already have their bilateral and other collaborations, make the SDG3 GAP what the report calls their “first port of call” for such collaboration.
It’s not surprising then that, the Lusaka Agenda is once again being seen as the life raft that will smoothen choppy waters and push forward novel approaches of collaboration, alignment and accountability. And it is hoped that the boards of governing bodies will help sail it through. But the fact that repeatedly, it is the global agencies that are releasing catalytic funding to ensure that communities are consulted underlines that despite the Lusaka Agenda, and despite the SDG3 GAP’s commitment to a “bottom-up” approach, in reality, this is restricted to the government-level only. The bottom-up process of decision making as a priority or to invest in making it more inclusive in every way is not what engages governments much. It’s often seen as a programmatic activity just prior to a national consultation if at all rather than a continuous dialogue. Besides community-level initiatives, catalytic funding also supports other aspects critical for implementation like gender equity. For instance, the report presents a case study of training in Gender Based Violence (see below) and the funding for inter-sectoral committees, among other initiatives, in Costa Rica.
|
“I take away lots of information on domestic and gender-based violence. That within each there can be a solution, support, to raise one’s voice, to not remain silent and to say ‘no more domestic violence and gender violence’”. |
But in the long-term, for these interventions to be sustainable, the onus lies equally on the country governance as well from local, provincial right up to the national level to dedicate domestic resources for them rather than be donor-dependent.
Reinventing the Wheel?
There is a model of collaboration that does not get the attention it deserves. The Eastern Mediterranean is the only region whose multi-agency and multi-sectoral international collaboration can be an exemplar for others. This is the Regional Health Alliance comprising offices of no less than 17 UN agencies (Figure 6) including its host – the WHO’s Regional Office for the Eastern Mediterranean region (EMRO). The alliance formed in 2020 includes the same seven accelerator groups that are part of the global SDG3 GAP, with a gender advisory group, to which have been added other organizations working in the region in the area of health to fulfil SDG targets. These agencies/organizations include those involved in emergency response, migration and refugees given that nearly half of all people in the region must live with environmental threats and natural disasters and in countries riddled with long-term conflicts.
|
Figure 6 The Regional Health Alliance The Regional Health Alliance is hosted by WHO for the Eastern Mediterranean and comprises regional offices of: |
The countries of the Eastern Mediterranean region span the Middle East and North Africa, comprising countries that are largely seen as mired in poverty and/or regressive practices, and/or practising a religion barely tolerated in the rest of the world. Yet it is in this zone that the Regional Health Alliance is operational, the only one of its kind among the regions covered by the WHO Regional Offices. Considering that the migration as a constant, disasters brought on by climate change and the refugee burden that the region faces are also concerns across the globe, and that gender equity is a pressing concern with the push back against it, it would be instructive to study this model of a functional, multi-sectoral, multi-agency alliance that is dealing with the very polycrises that the world faces today.
Showing it can be done! – indigenous knowledge as a data tool
While there has been heartburn over a perceived lack of acknowledgment of indigenous knowledge systems at various fora such as the World Health Summit Regional Meeting for the Asia-Pacific – indigenous-people-in-the-spotlight and the 77th World Health Assembly’s side event on community empowerment, the SDG3 GAP process in Colombia has done it. In Colombia, catalytic funding to the WHO Country Office was directed towards fostering community dialogue on how to include customs of ancestral indigenous birth attendance into regulatory frameworks and the national health system. The collaboration also improved the monitoring, evaluation and generation of data to track SDG progress through a health information system, which means that the customs are recognized as tools for data collection, generating evidence, a narrative so dear to global health discourse. However, once again, this was initiated from catalytic funding.
Conclusion
The dependence on catalytic funding for many new innovations and critical services begs the question whether in some way the entire lens of what is often dubbed “funding envelope” needs to be turned inside out. It’s an issue that came up during the Global Fund Strategy Review as well. It’s also wryly amusing that the “significant benefit to co-designing (or co-preparing) projects with partner governments from the beginning” is now being realized. Better late than never! But that this process has to encompass civil society and communities is also important, something that was recognized at the 77th World Health Assembly (WHA): “Member States have agreed on a resolution on social participation in national health planning and implementation, which paves the way for people, communities, and civil society to have a stronger voice in influencing the decisions that affect their health and well-being.” Now, for the implementation! Less talk, more action, please, as African government representatives in health and finance discussing the future of financial sustainability in African health systems on the sidelines of the 77 WHA pointed out!
